
Achilles Tendinopathy
Achilles Tendinopathy is a condition that affects runners, athletes and other active people. Often characterised by a sharp or dull pain in their calf or heel area – either first thing in the morning or during a run or other exercise. This article will explain some potential causes of Achilles Tendinopathy, the different types of tendinopathy and appropriate methods of treatment and pain management.
To understand Achilles Tendinopathy, first we need to understand: What is the Achilles Tendon?
The achilles tendon is the thickest and strongest tendon in the body. It is approximately 15 cm long. A tendon is a structure that connects muscle to bone. The Achilles tendon attaches from three muscles: gastrocnemius, soleus and plantaris (seen in figure 11). It widens as it inserts on the back surface of the heel bone. The gastrocnemius fibres attach on the outer part of the heel bone and the soleal fibres attach on the inside portion of the heel bone. The Achilles tendon can absorb shock and recoil, releasing the energy as part of the strong push off force it provides during walking (Moore, Dalley & Agur 2014).
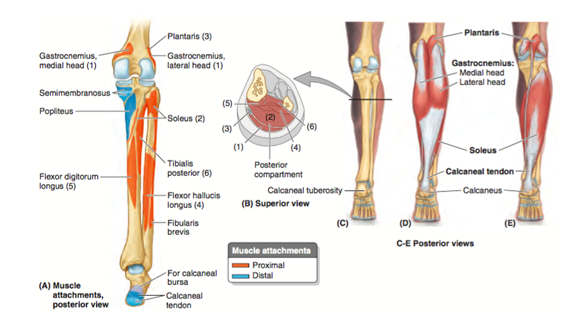
Figure 11
The achilles tendon is surrounded by an elastic sleeve which allows the tendon to move freely between surrounding tissue (Kiewet et al. 2013). The blood supply throughout the length of the tendon is poor. Poor blood supply may characterize the slow healing rate of the Achilles tendon following trauma (due to decreased access to nutrients and oxygen) (Carr & Norris 1989).
Three types of tendinopathy have recently been defined: reactive tendinopathy, tendon disrepair and degenerative tendinopathy (Cook & Purdham 2009)
What causes each of the types of Achilles Tendinopathy?
- Reactive Tendinopathy: sudden increase in load applied to tendon e.g. increased distance, speed or incline of physical activity or reduced rest between loads. There is no change to the structure of the tendon and is a reversible process (Cook & Purdam 2009).
- Tendon Disrepair: continual loading of a tendon in the reactive tendinopathy stage. The tendon and structure starts to breakdown and alter. There could be an increase in blood flow to and/or sensitivity of the area (Cook & Purdam 2009).
- Degenerative Tendinopathy: Chronic overloading of the tendon which results in the change of structure and function of the tendon, consequently causing it to be less capable of taking load. Its fibres become disorganized and it starts to break down (Cook & Purdam 2009). There is increased blood flow to and sensitivity of the area. This can lead to complete rupture of the tendon (Moore, Dalley & Agur 2014)

Why you might you think you have Achilles Tendinopathy?
You may have a tendinopathy of your Achilles tendon if you experience pain on the back part of your heel during walking, or weight bearing activity, especially when wearing rigid-soled shoes. It often occurs during repetitive activities like running and walking (Moore Dalley & Agur 2014).
Why you might you think you have an Achilles Tendon Rupture?
Rupture of the Achilles tendon is a significant injury. Individuals with this cannot raise the heel from the ground or balance on the affected side.
Walking is only possible when the limb is rotated outward, Bruising appears in the ankle bone region, and a lump usually appears in the calf due to shortening of the previously attached muscles, which are now unattached (Moore Dalley & Agur 2014).
What do we do to address and to treat the stages of Achilles tendinopathy?
Reactive Tendinopathy
During the reactive phase, the physiotherapist will work to reduce both tensile and compressive loads through the tendon, for example by placing a heel raise in your shoe (so that your foot is slightly plantarflexed).
Isometric exercise (exercise during which a muscle is activated but no movement of joints occur) is also great for pain relief yet ensures the maintenance of muscle strength. The exercise should be done in a position where the tendon is not compressed at all during the reactive phase (Rio et al. 2015).
Have you ever done a wall sit? Where you act as though you are sitting on a chair? This works the quadriceps muscle isometrically. It is a very strong exercise to increase the strength of the quadriceps but does so without having to move the muscle or the joints which it crosses at all. This is also similar to a plank. An isometric exercise for the core.
Please see figure 12 below which highlights an isometric exercise for the calf muscles (which act to plantar flex the foot). You should hold this position for as long as possible as high as possible where there is no pain:

Figure 12
Cook & Purdam (2012) suggest rather than stretching the Achilles musculature (gastrocnemius, soleus and plantaris), massage would be best to maintain muscle strength during the reactive phase to minimise risk of compression on the tendon.
During this stage it is important to rest the tendon as appropriately as possible to prevent the progression to the tendon disrepair stage when structural changes of the tendon occur (Cook and Purdam 2012).
It is important to gain advice from your physiotherapist regarding exactly how much rest should occur however, as there is a fine balance between offloading the tendon and immobilising it. Immobilisation can very rapidly result in weakness and reduction in function and overall performance. Your physiotherapist may prescribe exercise that places less stress through tension or compression of your Achilles tendon, for example through swimming or cycling. This is because repeatedly applying stress or trauma to the muscles, can cause friction between them, and results in an abnormal load of the Achilles tendon.
Disrepair/ Degenerative Tendinopathy
It is important to have an understanding of your tendons capacity to handle load. Working with the physiotherapist to document and map out when your symptoms are aggravated and when they are relieved is vital to your recovery.
Your physiotherapist can then help to plan an appropriate program of activity to control the recovery that will promote healing and prevent relapse. They will also be able to guide your increase in training intensity while allowing the tendon to adapt to load.
Another aspect of your rehabilitation program will include heavy-load exercise. The goal is to provide a strong, controlled, mechanical force to the Achilles tendon. This is usually achieved through eccentric (lengthening) muscle activity; for instance, a heel drop over a step. As tolerance of the exercise improves, the load is progressively increased (e.g. moving to single leg or adding weight) (Scott 2011)
Similarly to the addressing of contributing factors seen in plantar fasciitis and medial tibial stress syndrome above, the physiotherapist can also analyse your walking pattern and potential contributing factors to the excessive muscles soreness or excessive pronation of the foot including hip or core musculature. Also we must consider that the muscles contributing to the Achilles tendon are strong supinators of the foot and therefore have an effect of the arch of the foot and the entire biomechanics of the lower limb.
What Physiotherapy techniques do we offer to help?
It is important to remember each and every individual is different, and depending on the root cause of your presenting problem, the physiotherapists here at Therapia may use the following techniques to address and reverse your presentation, provided they are suitable to your condition:
- Muscle stretching and strengthening programs to address those contributing to poor foot and ankle alignment
- Mobilisation of tight structures contributing to the altered biomechanics of the lower limbs
- Dry Needling to promote healing, increase blood flow wash away toxins
- Arch strengthening
- Taping to decrease the tensile forces placed on the Achilles
- Motor pattern retraining and rehabilitation
- Individualised Pilates program
- Strain-Counter-Strain
- Footwear advice
Some exercises that benefit presentation and symptoms in these cases are:
- Calf Stretch in Tabletop
- Spiky Ball Release of Plantar Foot
- Hamstring Stretch in Standing

Please note that fibres of the Achilles tendon pass behind the back of the heel, and blend into the plantar fascia. This increased tension can cause inflammation either at the medial attachment site or within the plantar fascia itself.
There is a very distinct overlap between these conditions. Please make an appointment with us (link below) to find out more!
Disclaimer
If you are experiencing heel or ankle pain or have experienced heel or ankle pain in the past it is highly advised that you see your physio before starting any specific form of exercise to treat the symptoms.
The exercises listed above are an indication of what a heel/ankle exercise program would involve and are not recommended for anyone experiencing symptoms without first being assessed or speaking with a physio.
Book Appointment



