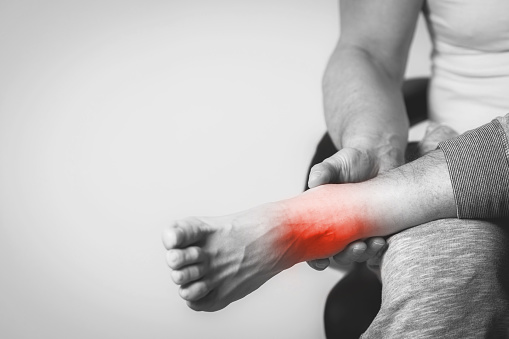
Ankle Sprains
Have you experienced ankle sprains?
The team at Therapia Physiotherapy & Pilates is here to help!
Ankle sprains are a common musculoskeletal injury, particularly amongst people who play sport. There are three main types of ankle sprain: lateral (outside), medial (inside) and high (between the two bones in your leg). Ankle sprains occur when a ligament in the ankle is stretched beyond its elastic threshold, which results in a partial or complete tear of the structure.
Anatomy
Ligaments comprise collagen and elastin fibres, proteoglycans plus water. The collagen is crimped and arranged into longitudinal, parallel bundles that transmit force. The elastin is elastic, usually returning to its original shape if/when deformed. The proteoglycans bind with the water and make a gel-like, spongy and resilient matrix.
The outside of your ankle has three ligaments: 1. anterior talofibular ligament (ATFL), 2. calcaneofibular ligament (CFL) and 3. posterior talofibular ligament (PTFL). ATFL sprains occur more frequently than CFL and PTFL sprains.

The inside of your ankle has four ligaments: 1. anterior tibiotalar ligament (ATTL), 2. tibionavicular ligament (TNL), 3. tibiocalcaneal ligament (TCL) and 4. posterior tibiotalar ligament (PTTL).
The area between the two bones in your leg also has four ligaments: 1. anterior-inferior tibiofibular ligament (AITFL), 2. interosseous ligament (IOL), 3. posterior-inferior tibiofibular ligament (PITFL) and 4. transverse tibiofibular ligament (TTFL).
Mechanism of Injury
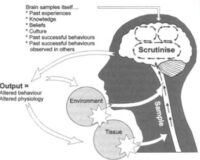
As mentioned above, ankle sprains occur when a ligament in the ankle is stretched beyond its elastic threshold, which results in a partial or complete tear of the structure. The crimped collagen fibres progressively uncrimp (reversible) then stretch (reversible) then fail/rupture (irreversible), with the tear occurring either in the middle or at either end of the ligament.
Lateral ankle sprains, specifically ATFL sprains, are the most common. They occur when your ankle undergoes excessive inversion (inwards) with plantarflexion (toes down). Medial ankle sprains occur when the ankle bone undergoes excessive eversion (outwards) and high ankle sprains with excessive rotation with dorsi flexion (toes up).

What symptoms are associated with an ankle sprain?
Patients with ankle sprains tend to experience an acute onset of ankle pain +/- swelling +/- bruising secondary to an unusual ankle movement (often whilst playing sport, e.g. tackle, stumble etc.) +/- an audible ‘pop’. They may also report a history of ankle instability &/or sprains +/- pins & needles, numbness &/or a sensation of cold.
What will an initial assessment for an ankle sprain involve?
Initial assessment for an ankle sprain involves taking a detailed patient history, observing your posture and gait pattern, testing your ankle range of movement plus palpation. Patients with ankle sprains tend to present with decreased weight-bearing in standing, an antalgic or ’painful’ walk, decreased, painful range of movement and ligament tenderness +/- swelling +/- bruising. The assessment also includes special tests to constrain which ligaments are involved and the grade of sprain +/- a neurological assessment (if pins & needles &/or numbness) +/- a pulse assessment (if a sensation of cold). Your ankle will also be checked for any associated fractures.
2 of the most common types of test are the Talar Tilt Test (lateral & medial) and the Squeeze Test (high).

What will physiotherapy treatment for an ankle sprain involve?
Physiotherapy treatment will be individualised to reflect the grade of your ankle sprain plus your personal goals, with reference to the ligament healing phases. Grade I (mild) to II (moderate) ligament sprains are treated conservatively and should resolve within weeks to months. Grade III (severe) ligament sprains may require surgical intervention and, as such, will take longer to heal.
Inflammatory Phase (0-3x days)
-
Patient education
-
RICE – rest, ice, compression & elevation
-
Anti-inflammatory cream +/- non-steroidal anti-inflammatories (NSAIDs)
-
Taping +/- brace +/- moon boot +/- crutches
-
Home exercise program (HEP) – gentle ankle ROM exercises (e.g. ankle ABCs) & calf stretches
Proliferative Phase (4-10x days)
-
Manual therapy – joint &/or neural mobilisation, STM, dry needling etc.
-
Progression of the HEP – strength, functional stability plus balance & proprioception exercises (e.g. theraband exercises, walking & single leg stand practice)
-
Paced return to activities of daily living
Remodelling Phase (11-21x days)+
-
Progression of manual therapy
-
Progression of the HEP – strength, functional stability plus balance & proprioception exercises (e.g. jumping >> hopping >> bounding exercises, stair climbing & star excursions)
- Paced return to sport

If you’re having issues with your ankles and would like to consult one of our physios feel free to give us a call anytime on 8221 5011 or send us an email at info@therapia.com.au.
You can book in for an appointment with one of our amazing practitioners through the link below.
Book Appointment
We look forward to seeing you soon!
Disclaimer:
None of the information in this article is a replacement for proper medical advice. Always consult with a medical professional for advice regarding your individual injury.